Table of Contents
Introduction
Free feeding, also known as demand feeding or responsive feeding, is a feeding method for infants in which the baby is fed whenever they show signs of hunger, rather than being fed on a schedule. With this method, the baby is allowed to determine how often and how much they want to feed based on their individual needs and hunger cues.
Free feeding is often recommended for breastfeeding mothers, as it helps establish and maintain a good milk supply. It allows the baby to feed as often as they need to obtain the optimal amount of breast milk. Free feeding can also be used with bottle-fed babies.
The American Academy of Pediatrics recommends responsive feeding, which is a form of free feeding that involves paying close attention to the baby’s hunger signs and providing them with appropriate amounts of food. This method can help promote healthy eating habits and weight gain in babies, as it encourages them to eat when they are hungry and stop eating when they are full.
The signs when a child is hungry: the child turns his head towards the mother and sucks his hand.

It’s important to note that while free feeding can be a beneficial feeding method for many infants, it may not be appropriate for all babies. Most mothers think such a way: if a baby cries – it is a sign that he is hungry. Unfortunately, a baby’s cry is not always an indicator of hunger. Children who have suffered birth injuries or have various diseases often cry.
Babies cry as a way of communicating their needs or discomfort since they are unable to express themselves through language. Crying is a normal and natural part of infant behavior and can indicate various things. Here are some common reasons why babies cry.
Everything about crying:
- Hunger: Hunger is one of the most common reasons for a baby to cry. If it’s been a while since the last feeding, your baby may be signaling that they are hungry.
- Sleepiness: Babies can become fussy when they are tired. Helping them establish a sleep routine and recognizing their sleepy cues can be helpful.
- Dirty Diaper: A wet or soiled diaper can be uncomfortable for a baby. Regular diaper checks and changes are essential.
- Discomfort or Pain: Babies may cry if they are uncomfortable due to factors such as tight clothing, a hair wrapped around a toe or finger, or a skin irritation.
- Need for Burping: If your baby has swallowed air during feeding, they may need to be burped to release the gas, preventing discomfort.
- Overstimulation: Too much noise, activity, or visual stimulation can overwhelm a baby. Sometimes they cry as a way of expressing their need for a quieter and calmer environment.
- Wanting to Be Held: Babies often crave physical contact and comfort. Sometimes, they may simply want to be held, rocked, or comforted by a caregiver.
- Teething: The process of teething can be uncomfortable for babies, and it may cause increased fussiness and crying.
- Illness or Discomfort: If your baby is sick or experiencing any form of discomfort, they may cry more than usual. It’s essential to monitor for other symptoms and consult with a healthcare professional if you are concerned.
- Colic: Some babies experience colic, which is characterized by intense, inconsolable crying, often in the evening. The exact cause of colic is not always clear, but it usually resolves on its own.
Resume:
It’s important to note that crying is a normal part of infancy, and it does not always signify a problem. Crying is a form of communication between a child and the world around him. However, if you are concerned about your baby’s crying, or if it is persistent and accompanied by other worrisome symptoms, it’s crucial to consult your paediatrician. They can provide guidance and help rule out any underlying health issues.
A sign that free feeding is suitable for your baby is normal signs of his physical and mental health and normal weight gain. Parents should always consult with their healthcare provider to determine the best feeding method for their individual baby’s needs.
Feeding a child under the age of 6 months
A child under the age of 6 months should receive only breast milk. There is no physiological need to introduce additional liquids into his diet.
Breast milk contains about 90% water, which fully satisfies the baby’s fluid needs. The introduction of additional fluids in the form of water, tea, juices, and decoctions increases the risk of acute intestinal infections. It reduces the need for breast milk and the duration of breastfeeding.
Basic rules for successful breastfeeding:
- Before breastfeeding, it is essential to clean your baby’s nose and ensure that the nasal passages are free of mucus and crusts because a baby breathes exclusively through the nose while suckling.
- Attaching the child to the mother’s breast during the first hour of life in the absence of contraindications.
- Round-the-clock stay of a mother with a child.
- Proper attachment of the baby to the mother’s breast.
- Do not give your child under 6 months of age any other foods and liquids except for those cases that are predetermined by medical indications.
- Do not use pacifiers.
- The mandatory introduction of adequate complementary foods is from 6 months.
- Continued breastfeeding up to 1 year and, if possible, longer.
Assessment of correct Breastfeeding
Breastfeeding assessment is carried out at each mandatory medical preventive examination of the child. Mothers can do this assessment by themselves.
It is necessary: a) to assess whether the baby is correctly attached to the mother’s breast and b) to determine the effectiveness of suckling.
Signs of the correct attachment of the child to the mother’s breast:
– the head and body of the child are in the same plane;
– the child`s body is pressed against the mother, facing the chest, the nose is opposite the nipple;
– the mother supports the whole body of the child from below, and not just his head and shoulders;
– the mother supports the breast from below with her fingers, while the index finger is below and the thumb is above (fingers should not be close to the nipple);
– first, the mother should touch the nipple to the baby’s lips and wait until the baby opens its mouth wide, and then quickly bring the baby closer to the breast, directing his lower lip below the nipple so that the baby captures the lower part of the areola;
– the position of the mother should be comfortable for her;
– the duration of feeding should not exceed 20 minutes. During this time, the child should not be allowed to fall asleep;
– If, after feeding, the mother has milk left, then its remains are decanted into a sterile dish. The most effective way to suck milk is with a vacuum apparatus (breast pump).
– It is necessary to store expressed milk in a refrigerator at a temperature not exceeding 4 C. Within 3-6 hours after expressing, milk can be used after heating to a temperature of 36-37 C. When stored for 6-12 hours – pasteurisation (water bath 65-75 C for 30 minutes). More than 12 hours – milk is sterilised (boiling in a water bath for 3-5 minutes).
– In order to prevent the formation of cracks and maceration of the nipples, the breast at the end of feeding should be washed with warm water and dried with a clean and soft diaper.
There are several types of breast pumps available on the market, designed to meet the varying needs of breastfeeding mothers. Here are the main types:
- Manual Breast Pumps:
These pumps require the user to manually operate a lever or handle to create suction.
They are usually compact, portable, and less expensive than electric pumps.
Manual pumps are suitable for occasional use or for mothers who express milk infrequently.
- Electric Breast Pumps:
These pumps are powered by electricity and automatically create suction to express milk.
Electric pumps are available in both single and double-pump models.
They are suitable for mothers who need to express milk regularly, such as working mothers.
- Double Electric Breast Pumps:
These pumps have two pumping mechanisms, allowing mothers to express milk from both breasts simultaneously.
Double pumping can save time and may stimulate milk production more effectively.
- Hospital-Grade Breast Pumps:
Hospital-grade pumps are high-powered electric pumps designed for frequent and prolonged use.
Mothers with premature babies, low milk supply, or specific medical conditions often use them.
These pumps are usually more expensive and may be available for rent.
- Wearable or Hands-Free Breast Pumps:
These pumps are designed to be worn discreetly and allow mothers to express milk without holding the pump.
They often fit inside a bra, providing more freedom of movement.
Wearable pumps are typically electric and rechargeable.
- Battery-Powered Breast Pumps:
Battery-powered pumps offer portability, making them suitable for use in situations where an electrical outlet may not be readily available.
Some electric pumps also have a battery-powered option.
- Hybrid or Combination Pumps:
These pumps can be used as both electric and manual pumps, providing flexibility for different situations.
Users can switch between electric and manual modes as needed.
Closed System vs. Open System Pumps:
Closed system pumps have a barrier between the milk collection kit and the pump motor, preventing milk from entering the pump mechanism. This design helps maintain hygiene.
Open-system pumps do not have a barrier, and there’s a possibility of milk entering the pump. These pumps require more thorough cleaning to prevent contamination.
When choosing a breast pump, it’s essential to consider factors such as your breastfeeding goals, frequency of use, budget, and personal comfort preferences. Consulting with a healthcare professional or a lactation consultant can also provide valuable guidance in selecting the right pump for your specific needs.
Determining the effectiveness of suckling:
When breastfeeding, the child himself regulates the amount of food he needs. If necessary, carry out control feeding: Weigh the baby before and after feeding. The difference in weight will correspond to the amount of milk sucked from the breast.
If the child sucks out an insufficient amount of milk, and also if he is sick or his mother is sick, then he is fed or supplemented with expressed human milk (it is recommended from a spoon so that he does not refuse the breast in the future).
Signs that your baby is not getting enough breast milk:
- Weight gain of less than 500 g per month;
- The child’s urination is less than 6 times a day; the urine is yellow and concentrated with a pungent odour.

Age periods when a baby needs more breast milk:
3 weeks; 6 weeks; 3 months.
This is predetermined by the intensive growth of the child during these age periods. It needs more frequent breastfeeding and should not be the reason for introducing milk mixtures into the child’s diet.
Lactation crises of mother:
During the period of breastfeeding, the mother may experience lactation crises. This is a temporary decrease in the amount of milk for no apparent reason, which lasts an average of 3-4 days and has a reverse character. It is necessary to inform the mother about the possibility of such crises, which may cause a temporary decrease in the amount of milk. During this period, the mother needs psycho-emotional support and rest.
Consulting a mother on the nutrition of a child under 6 months of age
- If the mother is ill with acute respiratory illness, breastfeeding should be continued. Breastfeeding should be stopped if the mother is taking medicines that, according to the instructions for use, are contraindicated for mothers who are breastfeeding.
- If a breastfeeding assessment reveals that the baby is not receiving enough milk, it is important to determine the possible cause and advise the mother:
- if breastfeeding is less than 8-10 times a day, the mother should be advised to increase the frequency of feedings;
- adhere to the principles of feeding at the request of the child, feeding at night;
- if the baby is not properly attached to the breast or is sucking ineffectively, it is important to teach the mother how to properly attach the baby to the breast;
- If the child receives other foods or drinks, it is necessary to advise the mother to breastfeed more often, reduce portions of other foods or drinks and subsequently refuse them;
- it is necessary to recommend that the mother eat well and involve other family members in caring for the child to ensure that she gets adequate rest;
- give up pacifiers and pacifiers.
Peculiarities of Feeding and Nutrition of a Child Aged 6-12 months: Сomplementary Food
At the age of 6 months, breast milk remains the main product for the child, but there is a need to expand the child’s diet and introduce additional products (complementary foods) into it. Breast milk at the age of 6 months can no longer satisfy the child’s need for calories and micronutrients, primarily iron, to ensure its normal development.
Complementary food is food products that are added to breast milk (or formula in the case of artificial feeding) to a child in the first year of life.
Rules for introducing complementary foods:
- Complementary feeding should be introduced while breastfeeding is continued.
- Complementary feeding should be given when the child is active and hungry, preferably during breakfast or lunch.
- Complementary feeding is given after a short period of breastfeeding (in the case of artificial feeding, a small amount of formula).
- During feeding, the child should be in an upright position, in a comfortable position in the mother’s arms or lap, or in a special highchair.
- Complementary foods should be given with a spoon. Each subsequent new complementary feeding product must consist of one ingredient and be given to the child for at least 5 days, after which mixed complementary feeding from these products can be given.
- To make it easier for a child to get used to new foods, it is recommended to add breast milk to complementary foods.
Practical takeaways – How do you implement complementary food in a child’s daily nutrition?
Complementary feeding should be started by placing a small amount of food on the tip of a teaspoon. Hold the spoon so that the child can see it. Then, touch the child’s lips with a spoon so that some of the product remains on his lips. Only when the child opens his mouth should the spoon with food be put in the middle of the tongue.
Important! – Each complementary feeding product is introduced starting with one teaspoon and increasing gradually, 5-7 days before the entire portion, dividing it into 2 feedings.
The child himself will show that he is complete by turning his head away, pushing away the spoon, or without opening his mouth.
It is essential to explain to the mother that each child has his own individual scheme for introducing complementary foods regarding the pace of introduction of various complementary foods.
Every time the baby has received complementary foods, it is advisable to put him on the breast of the mother to finish eating with breast milk. This will help maintain lactation, and the baby will feel satisfied.
If a child refuses complementary feeding, there is no need to force-feed him, as the child may refuse all food altogether. You can offer a different product (of a different taste or consistency) or the same one but on a different day.
Whole, undiluted cow’s milk should not be given to children under 9 months of age (it is a factor in the development of iron deficiency anaemia).
During the period of introducing complementary foods, salt and spices should not be added to complementary foods. Suppose signs of poor tolerance to a complementary food product appear (dysfunction of the digestive system, allergic reactions, etc.). In that case, you should stop introducing this complementary food product and introduce another one.

Conclusion: What is Important to Remember About the Nutrition of Children Under 1 Year
Here are some important points to remember:
Breast Milk or Formula:
Breast milk is the best source of nutrition for infants, providing essential nutrients and antibodies. Exclusive breastfeeding is recommended for the first six months of life. Complementary feeding is introduced from 6 months.
If breastfeeding is not possible, infant formula is a suitable alternative. Choose a formula recommended by healthcare professionals.
Introduction of Complementary Foods:
Begin introducing solid foods around six months of age while continuing to breastfeed or provide formula.
A child under 8 months of age should receive complementary foods 3 times a day.
At the age of 9-11 months, complementary feeding is done 4 times a day.
At the age of 1 year, a child should receive a variety of complementary foods from each food group and be able to drink from a cup.
From about 9 months, the baby can grasp objects with the thumb and forefinger. It is necessary to offer him small pieces of complementary food during meals to feed himself with a spoon.
Start with iron-rich foods like iron-fortified infant cereals, pureed meats, and legumes.
Nutrient-Rich Foods:
Offer a variety of nutrient-rich foods to ensure a balanced diet. Include fruits, vegetables, whole grains, and protein-rich foods.
Provide a mix of textures as your baby progresses from purees to mashed and finely chopped foods.
Iron-Rich Foods:
Iron is crucial for the development of the baby’s brain and body. Introduce iron-rich foods early, such as fortified cereals, pureed meats, and beans.
Vitamin D Supplement:
Breastfed infants may need a vitamin D supplement since breast milk alone may not provide enough of this vitamin. Formula-fed infants typically receive sufficient vitamin D from a formula.
Limiting Added Sugars and Salt:
Avoid adding sugar or salt to your baby’s food.
Limit the intake of processed foods, which may contain hidden sugars and excessive salt.
Responsive Feeding:
Pay attention to your baby’s hunger and fullness cues. Allow them to eat at their own pace.
Respect their preferences and gradually introduce a wide variety of flavours and textures.
Water Intake:
Breast milk or formula provides the necessary fluids for infants. Water is generally not needed until they start eating solid foods, and even then, small sips are sufficient.
Safe Feeding Practices:
Always supervise your baby during feeding to prevent choking.
Introduce one new food at a time and wait a few days before introducing another to monitor for any adverse reactions.
Regular Checkups:
Schedule regular well-child checkups with a paediatrician to monitor growth, development, and nutritional needs.
Discuss any concerns or questions about your baby’s nutrition with your healthcare provider.
Remember that every baby is unique, and individual nutritional needs may vary. Consulting with a healthcare professional can provide personalized guidance based on your baby’s specific requirements and circumstances.
Nutrition For a Child Aged 1 to 3 Years
During this period, it is important to formulate in the child the principles of healthy eating, which will contribute to his healthy development and preservation of health.
Children over 1 year of age can eat food that adults eat from the family table.
The recommended number of feedings for a child from 1 year to 2 years is at least 5 times a day – 3 main and 2 additional meals.
In the 2nd and 3rd years of life, children receive food 4 times a day. Breaks between feedings are 4.5 – 3.5 hours.
Continue breastfeeding into the second year of life.
The child’s diet should be varied, with fresh vegetables and fruits daily.
Low-fat varieties of meat, fish, liver, and eggs are recommended.
The child should receive bread, cereals, pasta, potatoes, milk and fermented milk products, eggs, vegetable oil and butter.
Food should be soft, porridge-like, homogeneous consistency in the form of purees, soufflés, meatballs, steamed cutlets, and fruits and vegetables should be finely chopped. With the appearance of molars in children, food may have the same consistency as in adults.
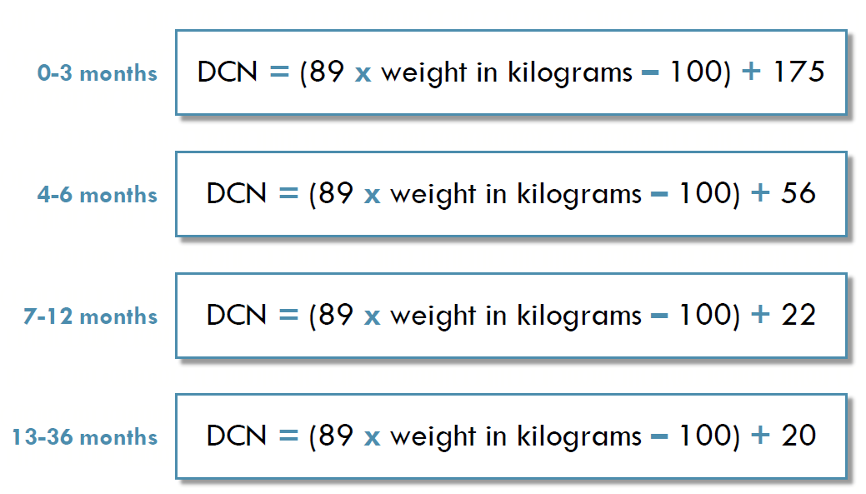
Practical Intake: Calculating a Child`s Calorie Needs DCN – Daily Calorie Needs
It is essential to remember that:
- Calories are a measure of energy.
- Calories provide fuel to the cells in the body.
- Each day provides our body with the energy it needs (your energy intake) and your body expends (uses up) this energy however it needs to.
- The energy taken in needs to be the same as the energy our body uses up for your weight to stay stable.
How can you assess a child’s caloric intake?
DCN calculation for 0 – to 36-month-olds
Tabl.1 Daily needs of young children in calories, proteins, fats and carbohydrates
| Age | Calories(kcal/day) | Protein(g/day) | Fats (g/day) | Carbohydrates(g/day) |
| 1–1,5 year | 1400 | 48 | 48 | 190 |
| from 1,5 to 3 years | 1600 | 53 | 65 | 210 |
| 3 to 5 years | 1800 | 65 | 65 | 270 |
| 5 to 7 years | 2000 | 70 | 70 | 290 |
In the next article, you will learn:
- What to do if a child is overweight or underweight.
- Where child’s do calories come from?
- Which foods should be minimised in a child’s diet, and what are healthier swaps?
- How can you start planning a child’s healthy diet?
You will be learning to assess how many calories a child may be consuming on a given day and how to begin planning a healthy diet. We’ll be giving you several practical examples together with helpful worksheets, including the “Child Daily Food Journal” and the “Child Daily Food Planner “.
You’ll know how to search for the nutritional facts in foods and compare a child’s actual caloric intake against their ideal caloric intake.
If you found this exploration of smart nutrition helpful, consider sharing it with friends and family. Your comments are valuable, and if you’re interested in professional child health creation services, learn more via this link.





