What are the main purposes of connective tissue?
Connective tissue (CT) occupies a special place in the body and is represented in all organs and tissues, making up more than half of the body weight. The variety of morphological structures that make up the connective tissue system determines a wide range of its functional properties and its indispensable participation in all processes occurring in the body [1, 2].
The quantitative predominance of the connective tissue system over other tissue systems of the body, on the one hand, and its participation in all processes occurring in the body, on the other, allows connective tissue to be considered the actual internal environment of the body.
Connective tissue performs a variety of vital functions, providing the structure of organs and tissues, the constancy of tissue permeability, water-salt balance, immunological protection, and support function. It is characterized by universality, specialization, multi-component, polymorphism of cellular systems, polyfunctionality, and high ability to adapt [3, 4]. Violation of the structure and function of connective tissue plays a considerable role in the development of chronic diseases of internal organs. In medicine, this is underestimated.
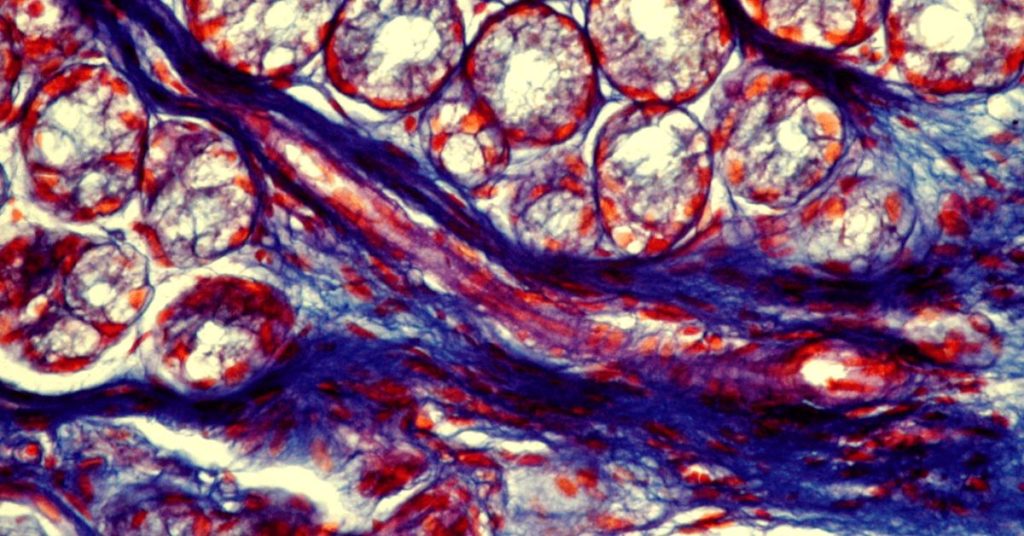
The source of connective tissue development is the mesenchyme, from which outwardly different tissues are formed: skin and bones, blood and lymph, smooth muscles, and cartilage. Connective tissue itself includes tissues of two types: fibrous connective tissue and connective tissue with specialized properties. In turn, fibrous connective tissue, according to the degree of development of fibers in the intercellular substance, can be loose and dense.
Loose unformed connective tissue is developed in all organs and forms their stroma, and is made up of extracellular matrix and collagenous, elastic, and reticular fibers.
Dense connective tissue, by the nature of the arrangement of fibers, is unformed (with a random arrangement of fibers), which is involved in the formation of the reticulate layer of the dermis, periosteum, and epicartilate, and decorated (with an orderly direction of the fibers) – ligaments, tendons, fascia, fibrous membranes.
Connective tissue with specialized properties is represented by mucous, adipose tissue, reticular tissues, blood, and lymph. Despite the external differences between these types of tissues, they all differ in the fantastic constancy of structural elements [5, 6].
Connective tissue consists of cellular elements and protein fibers. The major component of the matrix is a ground substance often crisscrossed by protein fibers. Cellular elements are represented by fibroblasts (FB), reticular cells, mast cells, plasma cells, and macrophages [3, 4].
Mast cells are a type of white blood cells located in connective tissue all through the body, they contain many granules rich in histamine and heparin and play an essential role in the allergic reactions of the body. The fibrous structures of the connective tissue are composed of collagen, elastic and reticular fibers. Cells and fibers are immersed in the ground substance CT, which consists of proteoglycans and glycoproteins, as well as mineral substances: Ca, K, Na, and Mg salts. From the blood plasma, immune antibodies, metabolites, proteins, vitamins, hormones, and ions enter the ground substance.
V. Serov and A. Schechter [7] emphasize that the intercellular substance is an information system that, experiences regulatory influences from the cells of the connective tissue and, in turn, has the same effect on them and the cellular systems of other tissues and organs. Such an interaction is probably based on feedback, which maintains homeostasis in the body, as well as regulates the functions of the connective tissue and changes that occur during pathological processes. All components of the intercellular substance are in a close structural and functional relationship.
The ground substance of the connective tissue is mainly represented by proteoglycans. The core of the proteoglycan molecule is a protein filament to which glycosaminoglycan (GAG) molecules are attached on all sides. GAGs are heteropolysaccharide biopolymers consisting of disaccharide units linked by a glycosidic bond. The functions of GAGs are to ensure the maintenance of constant tissue permeability, water-salt balance, the protective properties of the secretions of the mucous glands, the stabilization of fibrous structures, the regulation of cell division, and the immune response.
There are two types of GAGs: sulfated and non-sulfated. Sulfated GAGs: chondroitin-4-sulfate (x-4-c), chondroitin-6-sulfate (x-6-c), dermatan sulfate, keratan sulfate, and heparan sulfate. Non-sulfated GAGs: hyaluronic acid, chondroitin.
Glycoproteins of the ground substance include fibronectin, chondronectin, laminin, and entactin. Fibronectin, which ensures the interaction of fibroblasts with fibrillar structures, exists in two forms: soluble (circulates in the cerebrospinal and amniotic fluid) and associated with the cell surface. There is a plasma and cellular form of fibronectin, which are products of separate genes. Plasma fibronectin plays an essential role in phagocytosis, carries out humoral control of the function of macrophages, and is an opsonization factor [3, 4, 8].
Laminin is a high-molecular structural basement membrane glycoprotein, insoluble in water, has pronounced immune properties, and is able to bind strongly to heparin and type IV collagen.
Entactin is a protein component of the basement membrane and connects the networks formed by collagens and laminins to each other.
Fibroblasts (FB) are the central specific connective tissue cells with high metabolic activity. They carry out the synthesis and secretion of collagen, elastic and reticular fibers, glycoproteins and proteoglycans, and enzymes. Fibroblasts regulate their microenvironment and epithelial-mesenchymal interaction, together with fibrous structures, create CT architectonics. The functional role of the FB cell membrane, which is a receptor zone that regulates the influence of various factors, including hormonal ones, is excellent. FB growth and collagen production are regulated by factors secreted by macrophages [3, 8, 9].
Macrophages play a leading role in providing the protective function of CT in the body. They are the first cells with which microbes that have entered the internal environment of the body interact. Macrophages absorb opsonized microbes, kill them, and activate and synthesize cytokines – TNF-α, IL-1β, IL-6, IL-8, IL-12, α-interferon, etc., which have an activating effect on new populations of cells migrating to the inflammatory focus – monocytes, neutrophils, natural killers [10].
The functions of macrophages are not limited to the capture and degradation of foreign particles. They present the processed antigen to the T-lymphocyte. Without this function of macrophages, specific recognition of a foreign antigen is impossible. In the next stage, the stage of interaction between T- and B-cells, macrophages mediate this process, acting as a cell that transmits a specific turn-on signal from the T-lymphocyte.
In addition, they produce a number of components of the complement system (factors C-2, C-3, C-4, C-5), lysozyme, prostaglandins, interferon, and differentiation factors necessary for bone marrow hematopoietic stem cells for their differentiation in the granulocytic direction [11, 12].
Plasma cells are a component of the loose CT and the lymphatic system. They are formed from B-lymphocytes and synthesize antibodies.
Reticular cells synthesize reticular and thin collagen fibers and phagocytize antigenic proteins, being fixed phagocytes. In addition, mast cells secreting histamine, prostaglandins, heparin, serotonin, and a number of enzymes were found in the connective tissue. Mast cells are involved in collagen metabolism by influencing the collagenase activity of other cells by activating procollagenase [1, 13, 14].
The versatility of CT is mainly due to the properties of collagen, which is its main element. Collagen makes up more than 30% of the total body weight and is found not only in the skin and skeletal tissues (40-50%) but also in the stroma of all internal organs (10% of their mass). Today, 28 types of collagen are already known (the main five types of collagen I, II, IIi; IV, V), differing from each other in composition, predominant location in organs and tissues, and in the source of formation.
It should be taken into account that the processes of collagen biodegradation and biosynthesis are closely interrelated with proteoglycans and CT glycoproteins. Collagen biodegradation is also carried out during the interaction of fibroblasts, macrophages, lymphocytes, tissue basophilic granulocytes, and other CT cells under the control of the endocrine and immune systems. It is the fibrous structures, mainly collagen, that determine the strength of various types of CT. The elasticity and extensibility of CT are determined by the presence of elastic fibers in it [5, 15].
Thus, the diversity and complexity of the morphology and functions of the connective tissue provide it with a central role in genetic processes and suggest the active participation of its main elements in the development of many types of pathology. The morphological and functional integrity of the body is primarily determined by the connective tissue, the various morphological and functional structures of which provide immunological and biochemical homeostasis.
We are talking about the unique role of connective tissue as a barrier that protects the body from the penetration of infectious agents. At the same time, they mean, firstly, the direct activity of some cellular elements of the connective tissue in the fight against pathogenic organisms (phagocytosis) and, secondly, the leading role of CT cells in the implementation of the body’s immunological defense (antibody biosynthesis) [14]. Through the blood, the connective tissue has constant, two-way connections with the bone marrow – monocytes and granulocytes come from it.
From blood monocytes in the connective tissue, macrophages are formed – residents, and in the vessels – migrating macrophages. Lymphocytes also enter the connective tissue with blood and lymph. In phagocytic cells, a complex of factors is formed that stimulates the proliferation and differentiation of lymphoid cells, and the functional activity of mature T- and B-lymphocytes [9, 12]. It is also known that the nature of stem cell differentiation is determined by the microenvironment created by CT cells [11]. In this regard, we can assume a significant influence of the structure and metabolism of connective tissue on the functioning of the immune system, and the functional activity of its individual links.
The relationships between the collagens and the immune indicators were investigated. They are carried out through the lymphocyte-macrophage-fibroblast triad. An increase in phagocytic activity of macrophages helps to maintain metabolism CT at an average level. In this regard, the lysosomal enzymes of macrophages that break down CT fibers are of particular importance. It was discovered that through them, a specific state of mobile equilibrium of macrophages with fibroblasts is formed. From other sites, macrophages have a stimulating effect on fibroblasts, which are the leading producers of collagen [16].
Furthermore, it can be assumed that the use of stimulators of the T-system of immunity makes it possible to stimulate phagocytosis through direct connections and thus weaken the fibrosis process. This assumption is confirmed by the results of experimental studies, which show that the nature of fibrotic changes in the liver of rats changed significantly when CCl4 was administered to animals durably stimulated with bacterial polysaccharides. Under the influence of the immunostimulator, the number and absorption capacity of Kupffer cells increased and sclerotic processes in the liver stroma were inhibited [17].
We can summarize that the connective tissue and the immune system function together and are subsystems of one single system – the system of homeostasis. They are responsible for maintaining the constancy of the internal environment within the body, protecting it from external aggressive factors.
In the following Chapters, we will discuss disorders of connective tissue and which factors influence the interaction of the immune system and connective tissue metabolism, as well as the impact of connective tissue metabolism disorders and immunological reactivity on the formation of the chronic inflammatory process in the gastrointestinal tract.
You can learn more in my next article about connective tissue disorders here. Please leave your comments below if you liked this article.
References:
1. Ozolinya A.Zh. Biochemical aspects of connective tissue reactivity. Riga “Zinatne”. 1986.: 82.
2. Slutsky L.I. Biochemistry of normal and pathologically altered connective tissue. – L., Medicine. Leningrad branch., 1969.-374C.
3. Grechanina E.Ya. Pesochina E.A., Grechanina Yu.B. Hereditary diseases of the connective tissue: a textbook for medical cadets.-Kh., 1998.-25C.
4. Royce, P. M., & Steinmann, B. (Eds.). (2003). Connective tissue and its heritable sorders: molecular, genetic, and medical aspects. John Wiley & Sons.
5. Zemtsovsky E.V. Connective tissue dysplasia of the heart.-St. Petersburg.-1998.-94C.
6. Kamrani P; Marston G; Jan A. Anatomy, Connective Tissue. (2022). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
7. Serov V, Shekhter A. Connective tissue (1981) . M., Medicine. 312.
8. Martynov A, Stepura O, Ostroumova O. Congenital dysplasia of connective tissue. Bulletin of the Russian Academy of Medical Sciences. 1998.: 2.: 47-54.
9. OpenStax, Connective Tissue Supports and Protects. OpenStax CNX. Dec 15, 2016 http://cnx.org/contents/fe382569-de99-4d07-a334-757fb577e488@5. © Dec 15, 2016.
10. Khaitov R.N. Interaction of Cells of the Immune System: physiological and medical Aspects of Immunity. (1999). Immunology.: 1.- 6-16.
11. Petrov R. Immunology.-M.: Medicine, 1987.-406.
12. Sokolov E. Clinical Immunology. Guide for doctors. – M.: Medicine, 1998.-272.
13. Polikar A., Kolle A. Physiology of normal and pathological Connective Tissue. – Novosibirsk.: “Science”.1966.-267C.
14. Slutsky L.I. Biochemistry of normal and pathologically altered Connective Tissue. – L., Medicine. Leningrad branch., 1969.-374C.
15. Steinmann B, Royce P, Syperti–Furga. Connective Tissue and its Heritable Disorders: Molecular, Genetic and Medical Aspects. Eds. P.m. Royce, B. Steinmann.- New York,1993.-351-407.
16. Yakovleva I. Particularities of Gastroduodenal Pathology in Adolescents with systemic Connective Tissue Dysplasia. (2006). Manuscript. Ukraine.: 286.
17. Kustina, S, Mayansky D. (1981). Effect of Kupffer cell stimulation on the development of experimental liver cirrhosis. Bulletin of Experimental Biology and Medicine. 9, 366-369.



Pingback: (2022) Does It Make Sense To Have Children Vaccinated By Law? Practical Recommendations | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) Impact Of Connective Tissue Disorders On The Formation Of Gastrointestinal Pathology In Children And Adolescents | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) Why Are Childhood Diseases Important? All Parents Should Know | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) What Vitamins Are Found In Vegetables? | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) Impact Of Connective Tissue Disorders On The Formation Of Gastrointestinal Pathology In Adolescents | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) Vegetables Are Optimal Energy Sources For The Human Body | Childhealthcreation.com | How To Grow A Healthy Child?
Pingback: (2022) Evidence-based Approaches To The Prevention Of Gastrointestinal Pathology In Children And Adolescents With Non-inflammatory Hereditary Connective Tissue Disorders | Childhealthcreation.com | How To Grow A Healthy Child?